Route of administration
A route of administration in pharmacology and toxicology is the path by which a drug, fluid, poison, or other substance is taken into the body.[1] Routes of administration are generally classified by the location at which the substance is applied. Common examples include oral and intravenous administration. Routes can also be classified based on where the target of action is. Action may be topical (local), enteral (system-wide effect, but delivered through the gastrointestinal tract), or parenteral (systemic action, but delivered by routes other than the GI tract). Route of administration and dosage form are aspects of drug delivery.
Contents
Classification[edit]
Routes of administration are usually classified by application location (or exposition).
The route or course the active substance takes from application location to the location where it has its target effect is usually rather a matter of pharmacokinetics (concerning the processes of uptake, distribution, and elimination of drugs). Exceptions include the transdermal or transmucosal routes, which are still commonly referred to as routes of administration.
The location of the target effect of active substances are usually rather a matter of pharmacodynamics (concerning e.g. the physiological effects of drugs[2]). An exception is topical administration, which generally means that both the application location and the effect thereof is local.[3]
Topical administration is sometimes defined as both a local application location and local pharmacodynamic effect,[3] and sometimes merely as a local application location regardless of location of the effects.[4][5]
By application location[edit]
Enteral/gastrointestinal[edit]
Administration through the gastrointestinal tract is sometimes termed enteral or enteric administration (literally meaning 'through the intestines'). Enteral/enteric administration usually includes oral[6] (through the mouth) and rectal (into the rectum)[6] administration, in the sense that these are taken up by the intestines. However, uptake of drugs administered orally may also occur already in the stomach, and as such gastrointestinal (along the gastrointestinal tract) may be a more fitting term for this route of administration. Furthermore, some application locations often classified as enteral, such as sublingual[6] (under the tongue) and sublabial or buccal (between the cheek and gums/gingiva), are taken up in the proximal part of the gastrointestinal tract without reaching the intestines. Strictly enteral administration(directly into the intestines) can be used for systemic administration, as well as local (sometimes termed topical), such as in a contrast enema, whereby contrast media is infused into the intestines for imaging. However, for the purposes of classification based on location of effects, the term enteral is reserved for substances with systemic effects.
Many drugs as tablets, capsules, or drops are taken orally. Administration methods directly into the stomach include those by gastric feeding tube or gastrostomy. Substances may also be placed into the small intestines, as with a duodenal feeding tube and enteral nutrition. Enteric coated tablets are designed to dissolve in the intestine, not the stomach, because the drug present in the tablet causes irritation in the stomach.
The rectal route is an effective route of administration for many medications, especially those used at the end of life.[7][8][9][10][11][12][13] The walls of the rectum absorb many medications quickly and effectively.[14] Medications delivered to the distal one-third of the rectum at least partially avoid the "first pass effect" through the liver, which allows for greater bio-availability of many medications than that of the oral route. Rectal mucosa is highly vascularized tissue that allows for rapid and effective absorption of medications.[15] A suppository is a solid dosage form that fits for rectal administration. In hospice care, a specialized rectal catheter, designed to provide comfortable and discreet administration of ongoing medications provides a practical way to deliver and retain liquid formulations in the distal rectum, giving health practitioners a way to leverage the established benefits of rectal administration.
Parenteral[edit]
Parenteral administration can be performed by injection, that is, using a needle (usually a hypodermic needle) and a syringe,[16] or by the insertion of an indwelling catheter.
Locations of application of parenteral administration include:
- central nervous system
- epidural (synonym: peridural) (injection or infusion into the epidural space), e.g. epidural anesthesia
- intracerebral (into the cerebrum) administration by direct injection into the brain. Used in experimental research of chemicals[17] and as a treatment for malignancies of the brain.[18] The intracerebral route can also interrupt the blood brain barrier from holding up against subsequent routes.[19]
- intracerebroventricular (into the cerebral ventricles) administration into the ventricular system of the brain. One use is as a last line of opioid treatment for terminal cancer patients with intractable cancer pain.[20]
- epicutaneous (application onto the skin). It can be used both for local effect as in allergy testing and typical local anesthesia, as well as systemic effects when the active substance diffuses through skin in a transdermal route.
- sublingual and buccal medication administration is a way of giving someone medicine orally (by mouth). Sublingual administration is when medication is placed under the tongue to be absorbed by the body. The word "sublingual" means "under the tongue." Buccal administration involves placement of the drug between the gums and the cheek. These medications can come in the form of tablets, films, or sprays. Many drugs are designed for sublingual administration, including cardiovascular drugs, steroids, barbiturates, opioid analgesics with poor gastrointestinal bioavailability, enzymes and, increasingly, vitamins and minerals.
- extra-amniotic administration, between the endometrium and fetal membranes
- nasal administration (through the nose) can be used for topically acting substances, as well as for insufflation of e.g. decongestant nasal sprays to be taken up along the respiratory tract. Such substances are also called inhalational, e.g. inhalational anesthetics.
- intra-arterial (into an artery), e.g. vasodilator drugs in the treatment of vasospasm and thrombolytic drugs for treatment of embolism
- intra-articular, into a joint space. It is generally performed by joint injection. It is mainly used for symptomatic relief in osteoarthritis.
- intracardiac (into the heart), e.g. adrenaline during cardiopulmonary resuscitation (no longer commonly performed)
- intracavernous injection, an injection into the base of the penis
- intradermal, (into the skin itself) is used for skin testing some allergens, and also for mantoux test for tuberculosis
- intralesional (into a skin lesion), is used for local skin lesions, e.g. acne medication
- intramuscular (into a muscle), e.g. many vaccines, antibiotics, and long-term psychoactive agents. Recreationally the colloquial term 'muscling' is used.[21]
- intraocular, into the eye, e.g., some medications for glaucoma or eye neoplasms
- intraosseous infusion (into the bone marrow) is, in effect, an indirect intravenous access because the bone marrow drains directly into the venous system. This route is occasionally used for drugs and fluids in emergency medicine and pediatrics when intravenous access is difficult. Recreationally the colloquial term 'boning' is used.[21]
- intraperitoneal, (infusion or injection into the peritoneum) e.g. peritoneal dialysis
- intrathecal (into the spinal canal) is most commonly used for spinal anesthesia and chemotherapy
- Intrauterine
- intravaginal administration, in the vagina
- intravenous (into a vein), e.g. many drugs, total parenteral nutrition
- Intravesical infusion is into the urinary bladder.
- intravitreal, through the eye
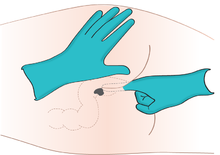
- Subcutaneous (under the skin).[22] This generally takes the form of subcutaneous injection, e.g. with insulin. Skin popping is a slang term that includes subcutaneous injection, and is usually used in association with recreational drugs. In addition to injection, it is also possible to slowly infuse fluids subcutaneously in the form of hypodermoclysis.
- transdermal (diffusion through the intact skin for systemic rather than topical distribution), e.g. transdermal patches such as fentanyl in pain therapy, nicotine patches for treatment of addiction and nitroglycerine for treatment of angina pectoris.
- perivascular administration (perivascular medical devices and perivascular drug delivery systems are conceived for local application around a blood vessel during open vascular surgery).[23]
- transmucosal (diffusion through a mucous membrane), e.g. insufflation (snorting) of cocaine, sublingual, i.e. under the tongue, sublabial, i.e. between the lips and gingiva, nitroglycerine, vaginal suppositories.
Topical[edit]
The definition of the topical route of administration sometimes states that both the application location and the pharmacodynamic effect thereof is local.[3]
In other cases, topical is defined as applied to a localized area of the body or to the surface of a body part regardless of the location of the effect.[4][5] By this definition, topical administration also includes transdermal application, where the substance is administered onto the skin but is absorbed into the body to attain systemic distribution.
If defined strictly as having local effect, the topical route of administration can also include enteral administration of medications that are poorly absorbable by the gastrointestinal tract. One poorly absorbable antibiotic is vancomycin, which is recommended by mouth as a treatment for severe Clostridium difficile colitis.[24]
Choice of routes[edit]
The reason for choice of routes of drug administration are governing by various factors:
- Physical and chemical properties of the drug. The physical properties are solid, liquid and gas. The chemical properties are solubility, stability, pH, irritancy etc.
- Site of desired action: the action may be localised and approachable or generalised and not approachable.
- Rate of extent of absorption of the drug from different routes.
- Effect of digestive juices and the first pass metabolism of drugs.
- Condition of the patient.
In acute situations, in emergency medicine and intensive care medicine, drugs are most often given intravenously. This is the most reliable route, as in acutely ill patients the absorption of substances from the tissues and from the digestive tract can often be unpredictable due to altered blood flow or bowel motility.
Convenience[edit]
Enteral routes are generally the most convenient for the patient, as no punctures or sterile procedures are necessary. Enteral medications are therefore often preferred in the treatment of chronic disease. However, some drugs can not be used enterally because their absorption in the digestive tract is low or unpredictable. Transdermal administration is a comfortable alternative; there are, however, only a few drug preparations that are suitable for transdermal administration.
Desired target effect[edit]
Identical drugs can produce different results depending on the route of administration. For example, some drugs are not significantly absorbed into the bloodstream from the gastrointestinal tract and their action after enteral administration is therefore different from that after parenteral administration. This can be illustrated by the action of naloxone(Narcan), an antagonist of opiates such as morphine. Naloxone counteracts opiate action in the central nervous system when given intravenously and is therefore used in the treatment of opiate overdose. The same drug, when swallowed, acts exclusively on the bowels; it is here used to treat constipation under opiate pain therapy and does not affect the pain-reducing effect of the opiate.
Oral[edit]
The oral route is generally the most convenient and costs the least.[25] However, some drugs can cause gastrointestinal tract irritation.[26] For drugs that come in delayed release or time-release formulations, breaking the tablets or capsules can lead to more rapid delivery of the drug than intended.[25] The oral route is limited to formulations containing small molecules only while biopharmaceuticals (usually proteins) would be digested in the stomach and thereby become ineffective. Biopharmaceuticals have to be given by injection or infusion. However, recent research (2018) found an organic ionic liquid suitable for oral insulin delivery (a biopharmaceutical) into the blood stream.[27]
Oral administration is often denoted "PO" from "per os", the Latin for "by mouth".
Local[edit]
By delivering drugs almost directly to the site of action, the risk of systemic side effects is reduced.[25] However, skin irritation may result, and for some forms such as creams or lotions, the dosage is difficult to control.[26]
Inhalation[edit]
Inhaled medications can be absorbed quickly and act both locally and systemically.[26] Proper technique with inhaler devices is necessary to achieve the correct dose. Some medications can have an unpleasant taste or irritate the mouth.[26]
Inhalation by smoking a substance is likely the most rapid way to deliver drugs to the brain, as the substance travels directly to the brain without being diluted in the systemic circulation.[28] The severity of dependence on psychoactive drugs tends to increase with more rapid drug delivery.[28]
Parenteral[edit]
The term injection encompasses intravenous (IV), intramuscular (IM), subcutaneous (SC) and intradermal (ID) administration.[29]
Parenteral administration generally acts more rapidly than topical or enteral administration, with onset of action often occurring in 15–30 seconds for IV, 10–20 minutes for IM and 15–30 minutes for SC.[30] They also have essentially 100% bioavailability and can be used for drugs that are poorly absorbed or ineffective when they are given orally.[25] Some medications, such as certain antipsychotics, can be administered as long-acting intramuscular injections.[31] Ongoing IV infusions can be used to deliver continuous medication or fluids.[32]
Disadvantages of injections include potential pain or discomfort for the patient and the requirement of trained staff using aseptic techniquesfor administration.[25] However, in some cases, patients are taught to self-inject, such as SC injection of insulin in patients with insulin-dependent diabetes mellitus. As the drug is delivered to the site of action extremely rapidly with IV injection, there is a risk of overdose if the dose has been calculated incorrectly, and there is an increased risk of side effects if the drug is administered too rapidly.[25]
Research[edit]
Neural drug delivery is the next step beyond the basic addition of growth factors to nerve guidance conduits. Drug delivery systems allow the rate of growth factor release to be regulated over time, which is critical for creating an environment more closely representative of in vivo development environments.[33]
Drugs are introduced into the body by several routes. They may be
- Taken by mouth (orally)
- Given by injection into a vein (intravenously, IV), into a muscle (intramuscularly, IM), into the space around the spinal cord (intrathecally), or beneath the skin (subcutaneously, sc)
- Placed under the tongue (sublingually) or between the gums and cheek (buccally)
- Inserted in the rectum (rectally) or vagina (vaginally)
- Placed in the eye (by the ocular route) or the ear (by the otic route)
- Sprayed into the nose and absorbed through the nasal membranes (nasally)
- Breathed into the lungs, usually through the mouth (by inhalation) or mouth and nose (by nebulization)
- Applied to the skin (cutaneously) for a local (topical) or bodywide (systemic) effect
- Delivered through the skin by a patch (transdermally) for a systemic effect
Each route has specific purposes, advantages, and disadvantages.
Oral route
Many drugs can be administered orally as liquids, capsules, tablets, or chewable tablets. Because the oral route is the most convenient and usually the safest and least expensive, it is the one most often used. However, it has limitations because of the way a drug typically moves through the digestive tract. For drugs administered orally, absorption may begin in the mouth and stomach. However, most drugs are usually absorbed from the small intestine. The drug passes through the intestinal wall and travels to the liver before being transported via the bloodstream to its target site. The intestinal wall and liver chemically alter (metabolize) many drugs, decreasing the amount of drug reaching the bloodstream. Consequently, these drugs are often given in smaller doses when injected intravenously to produce the same effect.
When a drug is taken orally, food and other drugs in the digestive tract may affect how much of and how fast the drug is absorbed. Thus, some drugs should be taken on an empty stomach, others should be taken with food, others should not be taken with certain other drugs, and still others cannot be taken orally at all.
Some orally administered drugs irritate the digestive tract. For example, aspirin and most other nonsteroidal anti-inflammatory drugs (NSAIDs) can harm the lining of the stomach and small intestine to potentially cause or aggravate preexisting ulcers. Other drugs are absorbed poorly or erratically in the digestive tract or are destroyed by the acid and digestive enzymes in the stomach.
Other routes of administration are required when the oral route cannot be used, for example:
Injection routes
Administration by injection (parenteral administration) includes the following routes:
A drug product can be prepared or manufactured in ways that prolong drug absorption from the injection site for hours, days, or longer. Such products do not need to be administered as often as drug products with more rapid absorption.
For the subcutaneous route, a needle is inserted into fatty tissue just beneath the skin. After a drug is injected, it then moves into small blood vessels (capillaries) and is carried away by the bloodstream. Alternatively, a drug reaches the bloodstream through the lymphatic vessels (see Figure: Lymphatic System: Helping Defend Against Infection). Protein drugs that are large in size, such as insulin, usually reach the bloodstream through the lymphatic vessels because these drugs move slowly from the tissues into capillaries. The subcutaneous route is used for many protein drugs because such drugs would be destroyed in the digestive tract if they were taken orally.
Certain drugs (such as progestins used for hormonal birth control) may be given by inserting plastic capsules under the skin (implantation). Although this route of administration is rarely used, its main advantage is to provide a long-term therapeutic effect (for example, etonogestrel that is implanted for contraception may last up to 3 years).
The intramuscular route is preferred to the subcutaneous route when larger volumes of a drug product are needed. Because the muscles lie below the skin and fatty tissues, a longer needle is used. Drugs are usually injected into the muscle of the upper arm, thigh, or buttock. How quickly the drug is absorbed into the bloodstream depends, in part, on the blood supply to the muscle: The sparser the blood supply, the longer it takes for the drug to be absorbed.
For the intravenous route, a needle is inserted directly into a vein. A solution containing the drug may be given in a single dose or by continuous infusion. For infusion, the solution is moved by gravity (from a collapsible plastic bag) or, more commonly, by an infusion pump through thin flexible tubing to a tube (catheter) inserted in a vein, usually in the forearm. Intravenous administration is the best way to deliver a precise dose quickly and in a well-controlled manner throughout the body. It is also used for irritating solutions, which would cause pain and damage tissues if given by subcutaneous or intramuscular injection. An intravenous injection can be more difficult to administer than a subcutaneous or intramuscular injection because inserting a needle or catheter into a vein may be difficult, especially if the person is obese.
When given intravenously, a drug is delivered immediately to the bloodstream and tends to take effect more quickly than when given by any other route. Consequently, health care practitioners closely monitor people who receive an intravenous injection for signs that the drug is working or is causing undesired side effects. Also, the effect of a drug given by this route tends to last for a shorter time. Therefore, some drugs must be given by continuous infusion to keep their effect constant.
For the intrathecal route, a needle is inserted between two vertebrae in the lower spine and into the space around the spinal cord. The drug is then injected into the spinal canal. A small amount of local anesthetic is often used to numb the injection site. This route is used when a drug is needed to produce rapid or local effects on the brain, spinal cord, or the layers of tissue covering them (meninges)—for example, to treat infections of these structures. Anesthetics and analgesics (such as morphine) are sometimes given this way.
Sublingual and buccal routes
A few drugs are placed under the tongue (taken sublingually) or between the gums and teeth (buccally) so that they can dissolve and be absorbed directly into the small blood vessels that lie beneath the tongue. These drugs are not swallowed. The sublingual route is especially good for nitroglycerin, which is used to relieve angina, because absorption is rapid and the drug immediately enters the bloodstream without first passing through the intestinal wall and liver. However, most drugs cannot be taken this way because they may be absorbed incompletely or erratically.
Rectal route
Many drugs that are administered orally can also be administered rectally as a suppository. In this form, a drug is mixed with a waxy substance that dissolves or liquefies after it is inserted into the rectum. Because the rectum’s wall is thin and its blood supply rich, the drug is readily absorbed. A suppository is prescribed for people who cannot take a drug orally because they have nausea, cannot swallow, or have restrictions on eating, as is required before and after many surgical operations. Drugs that can be administered rectally include acetaminophen (for fever), diazepam (for seizures), and laxatives (for constipation). Drugs that are irritating in suppository form may have to be given by injection.
Vaginal route
Ocular route
Drugs used to treat eye disorders (such as glaucoma, conjunctivitis, and injuries) can be mixed with inactive substances to make a liquid, gel, or ointment so that they can be applied to the eye. Liquid eye drops are relatively easy to use but may run off the eye too quickly to be absorbed well. Gel and ointment formulations keep the drug in contact with the eye surface longer, but they may blur vision. Solid inserts, which release the drug continuously and slowly, are also available, but they may be hard to put in and keep in place.
Ocular drugs are almost always used for their local effects. For example, artificial tears are used to relieve dry eyes. Other drugs (for example, those used to treat glaucoma [see table Drugs Used to Treat Glaucoma], such as acetazolamide and betaxolol, and those used to dilate pupils, such as phenylephrine and tropicamide) produce a local effect (acting directly on the eyes) after they are absorbed through the cornea and conjunctiva. Some of these drugs then enter the bloodstream and may cause unwanted side effects on other parts of the body.
Otic route
Drugs used to treat ear inflammation and infection can be applied directly to the affected ears. Ear drops containing solutions or suspensions are typically applied only to the outer ear canal. Before applying ear drops, people should thoroughly clean the ear with a moist cloth and dry it. Unless the drugs are used for a long time or used too much, little of the drugs enter the bloodstream, so bodywide side effects are absent or minimal. Drugs that can be given by the otic route include hydrocortisone (to relieve inflammation), ciprofloxacin (to treat infection), and benzocaine (to numb the ear).
Nasal route
If a drug is to be breathed in and absorbed through the thin mucous membrane that lines the nasal passages, it must be transformed into tiny droplets in air (atomized). Once absorbed, the drug enters the bloodstream. Drugs administered by this route generally work quickly. Some of them irritate the nasal passages. Drugs that can be administered by the nasal route include nicotine(for smoking cessation), calcitonin (for osteoporosis), sumatriptan (for migraine headaches), and corticosteroids (for allergies).
Inhalation route
Drugs administered by inhalation through the mouth must be atomized into smaller droplets than those administered by the nasal route, so that the drugs can pass through the windpipe (trachea) and into the lungs. How deeply into the lungs they go depends on the size of the droplets. Smaller droplets go deeper, which increases the amount of drug absorbed. Inside the lungs, they are absorbed into the bloodstream.

VIDEO

PHOTO COURTESY OF JUSTIN KAPLAN, MD.
Relatively few drugs are administered this way because inhalation must be carefully monitored to ensure that a person receives the right amount of drug within a specified time. In addition, specialized equipment may be needed to give the drug by this route. Usually, this method is used to administer drugs that act specifically on the lungs, such as aerosolized antiasthmatic drugs in metered-dose containers (called inhalers), and to administer gases used for general anesthesia.
Nebulization route
Similar to the inhalation route, drugs given by nebulization must be aerosolized into small particles to reach the lungs. Nebulization requires the use of special devices, most commonly ultrasonic or jet nebulizer systems. Using the devices properly helps maximize the amount of drug delivered to the lungs. Drugs that are nebulized include tobramycin (for cystic fibrosis), pentamidine (for pneumonia caused by Pneumocystis jirovecii), and albuterol (for asthma attacks).
Side effects can include those that occur when the drug is deposited directly in the lungs (such as cough, wheezing, shortness of breath, and lung irritation), spread of the drug into the environment (possibly affecting people other than the one taking the drug), and contamination of the device used for nebulization (particularly when the device is reused and inadequately cleaned). Using the device properly helps prevent side effects.
Cutaneous route
Drugs applied to the skin are usually used for their local effects and thus are most commonly used to treat superficial skin disorders, such as psoriasis, eczema, skin infections (viral, bacterial, and fungal), itching, and dry skin. The drug is mixed with inactive substances. Depending on the consistency of the inactive substances, the formulation may be an ointment, cream, lotion, solution, powder, or gel (see Topical Preparations).
Transdermal route
Some drugs are delivered bodywide through a patch on the skin. These drugs are sometimes mixed with a chemical (such as alcohol) that enhances penetration through the skin into the bloodstream without any injection. Through a patch, the drug can be delivered slowly and continuously for many hours or days or even longer. As a result, levels of a drug in the blood can be kept relatively constant. Patches are particularly useful for drugs that are quickly eliminated from the body because such drugs, if taken in other forms, would have to be taken frequently. However, patches may irritate the skin of some people. In addition, patches are limited by how quickly the drug can penetrate the skin. Only drugs to be given in relatively small daily doses can be given through patches. Examples of such drugs include nitroglycerin (for chest pain), scopolamine (for motion sickness), nicotine (for smoking cessation), clonidine (for high blood pressure), and fentanyl (for pain relief).
Chemotherapy and other drugs are often given in combination with each other and can be given in different ways. The method of administering the drug is based on the actual disease diagnosed and the agent's effectiveness. Common methods include:
- Intravenous (IV)(into a vein)
- Oral(by mouth)
- Intramuscular (IM) injection (into a muscle)
- Subcutaneous (SC) injection (under the skin)
- Intrathecal Therapy (within the spinal canal)
Intravenous
The intravenous (IV) route is a common way of giving medicine, especially chemotherapy, directly into a vein.
How Does It Work?
Your nurse inserts a small plastic needle into one of the veins in your lower arm. You may feel discomfort when the needle is inserted into your vein, but the rest of the procedure should be painless. The drugs flow from a plastic bag through tubing into your bloodstream. Sometimes a syringe is used to push the drugs through the tubing. If you feel any pain or burning while undergoing therapy, let your nurse know right away.
Using a Central Line
Many patients find that drug therapy can be given more conveniently and comfortably through a central line (catheter) than a regular IV. Certain medications irritate the veins and make repeated IV placement difficult. Catheters can also be used to supply nutrition, other drugs and blood cells and can be used to take blood samples.
Short-term catheters are temporary access devices for giving drugs and are removed before you leave the hospital. They're put in place in your hospital room, usually with local anesthesia.
Long-term catheters (also called tunneled catheters, or "Hickman®," "Broviac®" or "Groshong®" catheters) can remain in place for weeks or months. To place the catheter, your doctor makes a small incision and threads the IV line — a long, thin tube — into the vein and under the skin to a second small incision at a distance from the first. (This distance helps prevent infection.) Most catheters are positioned on the chest wall. You may have a few stitches at one or both sites until the areas have healed. Small, clear dressings are changed frequently to prevent infection. Hospital or clinic staff will show you, your family members or caregivers how to clean and care for the central line.
Using a Port
Sometimes a port is implanted to access the vein. A port is a type of long-term catheter that's surgically implanted under the skin's surface on the upper chest wall. Once the site heals, no dressings are needed and no special home care is required. To deliver the drugs, the nurse inserts a needle through your skin to access the port. You can choose to have a local numbing cream applied to the injection site before the port is used. The port can be used to draw and supply blood as well as provide nutrition.
Using a PICC Line
Another option is a percutaneously inserted central venous catheter, more commonly referred to as a PICC or PIC line. This type of catheter — a long, thin, flexible tube — is inserted through a vein in the arm. Before the PICC's insertion, you'll be given a local anesthetic to numb your arm in the area between the elbow and shoulder. The doctor threads the PICC line through the skin into a vein in the arm until it reaches the superior vena cava just above the heart. The superior vena cava is one of the veins in the central venous system.
You'll need to have any long-term devise periodically flushed. Your doctor will give you a plan for how to have your device flushed as well as how often.
Oral
The oral method takes the form of a pill, capsule or liquid that you swallow. This is the easiest and most convenient method since it can be done at home. Thalidomide, lenalidomide and imatinib mesylate are examples of blood cancer drugs taken by mouth. The side effects of oral chemotherapy are similar to those from IV chemotherapy.
To take anticancer drugs by mouth at home, you must understand the drug dosage and frequency, any possible interactions with food and other drugs, storage and handling, and potential side effects. You must take these drugs exactly as prescribed. You may find that medication calendars, planners and timers set as reminders to take medications are useful.
Intramuscular Injection
Intramuscular drugs are injected into the muscle, usually in the arm, thigh or buttock. You'll feel a slight pinch, lasting a few seconds, as the nurse slips the needle through your skin and into the muscle.
Subcutaneous Injection
Subcutaneous drugs are injected into the tissue under the skin instead of into the muscle. You'll feel a slight pinprick as the nurse inserts the needle under your skin.
Intrathecal Therapy
Certain types of leukemia and lymphoma have a tendency to spread to the nervous system. To prevent or treat this, your doctor delivers the drugs directly into your spinal canal, which more effectively treats hard-to-reach spine and brain cells than chemotherapy drugs injected into a vein. This is known as an intrathecal drug delivery, meaning within the spinal canal, which is the space between the double-layered covering or lining of the brain and spinal cord. The lining is called the meninges.
How Does It Work?
When you undergo intrathecal therapy, your doctor performs a lumbar puncture (spinal tap) by inserting a needle into your spinal canal; this can be done with either local anesthesia or with sedation/anesthesia. He or she removes spinal fluid, which is examined for leukemic cells, and then injects fluid containing chemotherapy drugs, usually cytarabine or methotrexate.
If you need many treatments, your doctor may place a permanent device called an Omaya reservoir under your scalp. Once the Omaya reservoir is inserted, your treatments can be delivered through this device and you'll no longer need lumbar punctures. You'll be able to go home with the Omaya reservoir in place.
Some medications must be given by an intravenous (IV) injection or infusion. This means they’re sent directly into your vein using a needle or tube. In fact, the term “intravenous” means “into the vein.”
With IV administration, a thin plastic tube called an IV catheter is inserted into your vein. The catheter allows your healthcare provider to give you multiple safe doses of medication without needing to poke you with a needle each time.
In most cases, you won’t give yourself an intravenous medication. While you can take some infusion medications yourself at home, you’ll likely receive your therapy from a healthcare provider. Read on to learn about the two main tools used for IV administration — standard IV lines and central venous catheters — including why they’re used and what the risks are.
IV medication is often used because of the control it provides over dosage. For instance, in some situations, people must receive medication very quickly. This includes emergencies, such as a heart attack, stroke, or poisoning. In these instances, taking pills or liquids by mouth may not be fast enough to get these drugs into the bloodstream. IV administration, on the other hand, quickly sends a medication directly into the bloodstream.
Other times, medications may need to be given slowly but constantly. IV administration can also be a controlled way to give drugs over time.
Certain drugs may be given by IV administration because if you took them orally (by mouth), enzymes in your stomach or liver would break them down. This would prevent the drugs from working well when they’re finally sent to your bloodstream. Therefore, these drugs would be much more effective if sent directly into your bloodstream by IV administration.
Standard IV lines are typically used for short-term needs. For instance, they may be used during a short hospital stay to administer medication during surgery or to give pain medications, nausea medications, or antibiotics. A standard IV line can typically be used for up to four days.
With standard IV administration, a needle is usually inserted into a vein in your wrist, elbow, or the back of your hand. The catheter is then pushed over the needle. The needle is removed, and the catheter remains in your vein. All IV catheters are typically given in a hospital or clinic.
A standard IV catheter is used for two kinds of IV medication administration:
IV push
An IV “push” or “bolus” is a rapid injection of medication. A syringe is inserted into your catheter to quickly send a one-time dose of drug into your bloodstream.
IV infusion
An IV infusion is a controlled administration of medication into your bloodstream over time. The two main methods of IV infusion use either gravity or a pump to send medication into your catheter:
Pump infusion: In the United States, a pump infusion is the most common method used. The pump is attached to your IV line and sends medication and a solution, such as sterile saline, into your catheter in a slow, steady manner. Pumps may be used when the medication dosage must be precise and controlled.
Drip infusion: This method uses gravity to deliver a constant amount of medication over a set period of time. With a drip, the medication and solution drip from a bag through a tube and into your catheter.
Long-term medication treatment, such as chemotherapy or total parenteral nutrition, usually requires a central venous catheter (CVC) instead of a standard IV catheter. A CVC is inserted into a vein in your neck, chest, arm, or groin area.
CVCs can be used for a longer period of time than a standard IV line. A CVC can stay in place for several weeks or even months.
The three main types of CVCs include:
Peripherally inserted central catheter (PICC)
A PICC has a long line that sends medication from the area of insertion, through your blood vessels, all the way to a vein near your heart. A PICC is typically placed in a vein above your elbow in your upper arm.
Tunneled catheter
With a tunneled catheter, medication can be sent directly into blood vessels in the heart. One end of the catheter is placed into a vein in the neck or chest during a short surgical procedure. The rest of the catheter is tunneled through the body, with the other end coming out through the skin. Medications can then be given into that end of the catheter.
Implanted port
Like a tunneled catheter, an implanted port inserts a catheter into a vein in the neck or chest. This device is also placed during a short surgical procedure. But unlike a tunneled catheter, an implanted port is located completely beneath the skin. To use this device, a healthcare provider injects medication through the skin into the port, which sends the medication into the bloodstream.
Many different types of medications can be given by IV. Some of the drugs more commonly given by this method include:
- chemotherapy drugs such as doxorubicin, vincristine, cisplatin, and paclitaxel
- antibiotics such as vancomycin, meropenem, and gentamicin
- antifungal drugs such as micafungin and amphotericin
- pain medications such as hydromorphone and morphine
- drugs for low blood pressure such as dopamine, epinephrine, norepinephrine, and dobutamine
- immunoglobulin medications (IVIG)
While IV medication use is generally safe, it can cause both mild and dangerous side effects. Medications given intravenously act on the body very quickly, so side effects, allergic reactions, and other effects can happen fast. In most cases, a healthcare provider will observe you throughout your infusion and sometimes for a period afterward. Examples of IV side effects include:
Infection
Infection can occur at the injection site. To help prevent infection, the administration process must be done carefully using sterile (germ-free) equipment. An infection from the injection site can also travel into the bloodstream. This can cause a severe infection throughout the body.
Infection symptoms can include fever and chills, as well as redness, pain, and swelling at the injection site. If you have any symptoms of infection, call your doctor right away.
Damage to blood vessels and injection site
A vein can be damaged during injection or by the use of an IV catheter line. This can cause infiltration. When this occurs, medication leaks into surrounding tissue instead of going into the bloodstream. Infiltration can cause tissue damage.
IV administration can also cause phlebitis, or inflammation of the veins. Symptoms of both infiltration and phlebitis include warmth, pain, and swelling at the injection site. Call your doctor right away if you have any of these symptoms.
Air embolism
If air gets into the syringe or the IV medication bag and the line runs dry, air bubbles can enter your vein. These air bubbles can then travel to your heart or lungs and block your blood flow. An air embolism can cause severe problems such as heart attack or stroke.
Blood clots
IV therapy can cause blood clots to form. Clots can block important blood vessels and cause problems such as tissue damage or death. Deep vein thrombosis is one type of dangerous blood clot that IV treatment can cause.
IV drug administration is a fast, effective way to send medication into your bloodstream. If your doctor has prescribed it for you, they will likely explain the purpose and the process for your treatment. But if you have questions, be sure to ask. Your questions may include:
- How long will I need to have my IV treatment?
- Am I at high risk of any side effects?
- Can I receive my IV medication at home? Can I give it to myself?
Intravenous drug use is a method of introducing mind-altering substances into the body with an intravenous needle. The IV needle is used to pierce the skin to reach the vein and inject the substance. Drugs may also be introduced into the body by intramuscular or subcutaneous injection. With an intramuscular injection, the drug is introduced into the muscle, while a subcutaneous injection is done directly under the skin, without hitting the vein itself.
Common Slang Terms for IV Drug Use
To prevent detection from outsiders and law enforcement, IV drug users often use slang terms to describe this particular method of getting high. Common slang terms are “shooting up,” “pinning,” “jacking up,” “banging” and “slamming.” Common slang terms for IV drugs themselves include “smack” to describe heroin; “crank,” “meth,” “ice” and “glass” to refer to crystal methamphetamines; and “soda” to describe injectable cocaine.
*What Drugs Are Taken Intravenously?
The most common drugs used among IV users are:
- Heroin
- Cocaine
- Crystal methamphetamines
- Amphetamines
- Opiates
- Prescription drugs
Prescription drugs taken illegally by injection include everything from barbituates to hydrocodone. According to the statistics published on the National Institute of Drug Abuse website, nearly 16 million people in the United States have abused prescription drugs, using them for a purpose other than what they were prescribed for or going beyond the dosage and recommended method of administration.
How IV Drugs Are Used
The street drug in question is sold in crystal or powder form and then needs to be prepared before injection. The drug is usually dissolved in water on a spoon or the bottom of a soda can and sometimes heated, depending on the drug. Once the drug is properly mixed and dissolved, the user takes a small syringe and draws the solution through a ball of cotton and injects it.
Why Some Drug Users Prefer the Intravenous Method
Drug users who began with pills may have found the high is no longer what they expect so they turn to the intravenous method. IV drug use completely circumvents the digestive system so the high is almost immediate. Huffing and snorting can do damage to delicate mucous membranes and IV drug use avoids this. People with sensitive stomachs may also prefer the IV method.
However, there are serious dangers associated with this method, HIV infection being the most common. According to a published report, single unemployed males between the ages of 30 and 34 are the most at risk for needle-sharing related diseases such as HIV and hepatitis C.
Health Risks
Though the IV method may be preferred by some drug users, it can also cause serious health complications. The most common being:
- Increased risk of blood-borne disease. Though sexual intercourse is the number one HIV transmission method, intravenous drug use is a close second. According to the Centers for Disease Control (CDC), injection drug use is the cause of over 36 percent of AIDS cases in the US. In addition to this risk, IV drug use can also put the user at risk for the development of hepatitis C, another incurable blood-borne autoimmune disease.
- Infections. Staph infection is one of the deadliest skin infections and often associated with IV drug use. If your skin is dirty when you inject, the bacteria on your skin can transfer to your veins and develop into a bacterial infection. Subcutaneous injections can also cause bacterial infections to develop right under the skin.
- Abscesses. Another common health problem associated with IV drug users is skin abscesses. A skin abscess is a grouping of pus that develops because of a bacterial infection such as staph. These pustules are dark red and circular with red and swollen tenderness at the site.
- Collapsed veins. Whether you’re an IV drug user or a diabetic, the result is the same. If you continue to inject in the same site, your veins may eventually reject this and collapse. Though most intravenous drug users switch spots often to avoid this, it can still create lasting health problems.
- Increased chance of overdose. Since the high from the IV method of drug use is so immediate and bypasses all of your body’s detoxifying systems, the chances of overdose are much higher. According to a study published in the International Journal of Epidemiology, the users at highest risk for death by overdose are those who went through rehabilitation but left before finishing the program.
*Signs of Intravenous Drug Use
Worried a loved one is using drugs? Here are some common signs of IV drug use:
- Sudden neglect of responsibilities
- Neglect of personal hygiene
- Track marks on arms
- Wearing of long sleeves in warm weather (to hide marks)
- Swollen or puffy hands and feet
- Extreme hyperactivity or lethargy
- Bloodstained water or tissues
- Knotted pantyhose or shoestring (used as a tourniquet)
- Sudden withdrawal from usual activities
- Irritability or anxiety
- Borrowing or begging for money
Since some of these signs and symptoms may be related to a mental or physical illness, it is important not to accuse or act irrationally when confronting someone. Always be gentle in your approach.
Mitigating the Risk of Using Needles
Since IV drug use is so risky and addiction has such a stronghold on users, it’s important for addicts to understand their responsibilities when it comes to staying safe. Stopping all IV drug use is the ideal option; however, those who simply won’t stop use should aim to always use clean needles and never share mixing water with anyone. When it comes to getting clean needles, search for a needle exchange program in your area.
Seeking Treatment
Intravenous drug use can be a difficult habit to beat. Just remember, it didn’t start out as a habit. Maybe it was something you tried once with your friends or something you used to get through a tough semester of college. Whatever the reason for your drug use, there is plenty of help available to you.
If your business and social life is suffering, or if you’re struggling both financially and spiritually, it may be time to reach out to someone who understands. If you have any questions about IV drug use or how you can get treatment today, contact us. We can connect you with a treatment program that will work well for your current situation. Don’t waste another day; give us a call now.